Archived Content
This page is archived and provided for historical reference. The content is no longer being updated, and some of the information may have changed over time and could be outdated or inaccurate.

By Lauren Fordyce, Ph.D.
Understanding the way patients think and behave is critical for effective care. That theme is paramount in a workshop to be hosted by the Office of Behavioral and Social Sciences Research (OBSSR), in collaboration with the Behavioral and Social Science (BSS) Consortium for Medical Education. The workshop is designed to disseminate best practices and share the successes of more than 10 years of research from medical schools that have implemented behavioral and social sciences curricula into interprofessional health education throughout the United States.
The workshop, Integrating Behavioral and Social Sciences (BSS) into Health Education, will be held April 22, 2016, at the National Institutes of Health (NIH) campus in Bethesda, Maryland. Attendance is free, but registration is required.
Understanding theories and methods of behavior change is important for physicians to improve patient health
In 2004, the National Academies of Sciences, Engineering, and Medicine—Health and Medicine Division, formerly the Institute of Medicine (IOM), released the report, “Improving Medical Education: Enhancing the Behavioral and Social Science Content of Medical School Curricula,” which highlighted the importance of integrating BSS curricula into medical education.
For instance, the report noted that understanding the theories and methods of behavioral change are important tools for physicians to have in order to improve the life and health outcomes of their patients. Likewise, as awareness of health disparities and their effects grows throughout the United States, social science tools are valuable in helping health care professionals fully understand how social, economic, and cultural factors can influence health outcomes (Institute of Medicine 2004).
The report emphatically recommended to “Provide an integrated 4-year curriculum in the behavioral and social sciences. Medical students should be provided with an integrated curriculum in the behavioral and social sciences throughout the 4 years of medical school” (Institute of Medicine 2004:11).
Provide an integrated four year curriculum in the behavioral and social sciences
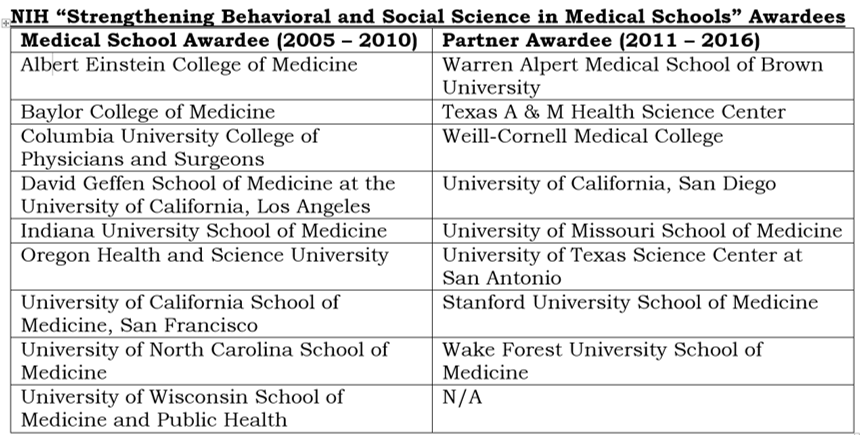
To this end, the NIH awarded Career Development Awards (K07s) to nine medical schools to develop, pilot, and disseminate BSS curricula throughout all four years of medical school in both the pre-clinical and clinical phases.
In the first round of funding (2005–2010), approximately 6,100 medical students were affected by the curricular innovations, and more than 120 dissemination activities were completed, including 19 peer-reviewed publications (Hollar et al., 2007).
Given the success of the intervention, the NIH invited all awardees to apply for an additional round of funding (2011–2016), with the added stipulation that renewing schools were required to include a new partner school to facilitate dissemination and innovation. Eight of the original schools were funded, and the new round of funding included a greater focus on interprofessional education, public health, resident training, and other curricula innovations.
Workshop to share methods and mechanisms for integrating social and behavioral science into health education
As the grant cycles conclude for the second round of funding, members of the BSS Consortium for Medical Education will gather later this month at an OBSSR-sponsored workshop to share methods and mechanisms for integrating BSS curricula into interprofessional health education. The workshop will focus on four themes:
- Innovations in Physician/Patient Communication
- Professional Development and Reflective Narrative Writing in BSS
- Interprofessional Education in the BSS
- Reflective Awareness and Practice
The presentations by principal investigators will be followed by a “reactor panel” featuring key stakeholders from the interprofessional health care education community, including representatives from the American Medical Association, the Accreditation Council for Graduate Medical Education, the American Association of Colleges of Pharmacy, the Association of American Medical Colleges, and the National Center for Interprofessional Practice and Education. The final panel will also include a response from Dr. Tom Inui, from Indiana University School of Medicine, who was one of the original members of the Committee on BSS in Medical Schools Curricula that produced the original 2004 IOM report.
Over the next few weeks, the OBSSR Connector will feature a series of posts highlighting some of the research of the BSS Consortium for Medical Education. The Consortium have published more than 100 peer-reviewed publications and participated in more than 400 dissemination activities including oral and poster presentations, workshops, student projects, and grants. We look forward to highlighting all the important work of the Consortium at the workshop later this month and on this site.
References
Hollar D, Satterfield JM, Carney PA, Graham M, Wimmers P, Swiderski DM, Skochelak SE, Dewey C, Litzelman DK, Stuber ML, Cross AW, Charon R, Chappelle KG, Marantz PR, & Naqvi Z. (2007) “The National Institutes of Health Social and Behavioral Science Consortium: An Introduction and Progress Report on Undergraduate Medical Education Curricular Innovations.” Annals of Behavioral Science and Medical Education 13(2):60-68.
Institute of Medicine (2004) Improving medical education: Enhancing the behavioral and social science content of medical school curricula. Washington, DC: The National Academies Press.
About the Author
Lauren Fordyce, Ph.D.
American Association for the Advancement of Science (AAAS) Science and Technology Policy Fellow
Dr. Lauren Fordyce is a medical anthropologist with a background in the anthropology of reproduction, women’s health, and migration. She received her M.A. and Ph.D. in cultural anthropology from the University of Florida. Her National Science Foundation–funded research examined ideas about risk in pregnancy among Haitian migrant women living in Miami, Florida. Most recently she has published manuscripts on social framings of risk in pregnancy; unintended pregnancy among Haitians in Miami; fetal death as tracked through vital statistics; and narratives of blame related to fetal and infant death. After completing her Ph.D., Dr. Fordyce spent five years teaching undergraduate anthropology courses at The University of North Carolina at Asheville, Bucknell University, and The University of North Carolina at Chapel Hill.
In the OBSSR, Dr. Fordyce is working on a number of projects, including: (1) shaping a new research agenda examining the links between education and health outcomes, (2) evaluating the OBBSR health disparities effort, and (3) collaborating with the medical school consortium to disseminate their efforts on enhancing behavioral and social sciences in medical education.
Photo Credit: shutterstock/ wavebreakmedia








